New! E-Learning: Link to patient setup tutorial
Installation and signal quality
Applications and Clinical benefits
The new reference in Cardiac Output monitoring
Why measuring Cardiac Output?
Cardiac Output (CO) is the amount of blood pumped by the heart in liters per min. It is the true "raison d'être" of the heart.
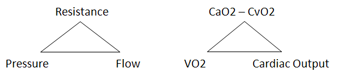
CO is a hemodynamic parameter that plays a key role in several physiological equilibriums. For instance: it is the dynamic force that generates arterial blood pressure by combination with the systemic vascular resistance (SVR). Another example is the close interaction between Co, oxygen consumption (VO2) and peripheral oxygen extraction described by the "Fick" equation.
As a result and for instance, systemic hypertension should not be managed without the knowledge of cardiac output because CO is a key contributor to the calculation of SVR which is essential in understanding and managing this pathology. Similarly, relying on VO2 only to evaluate the physiology of exercise is way too restrictive considering the importance of cardiac and peripheral parameters as potential limiting factors for human performance.
CO, Stroke Volume (SV) and their components (preload, contractility, afterload) need to be evaluated in dynamic manner. For instance, the rate of increase of SV and contractility during exercise differs considerably from a heart failure patient to an athlete. Abnormal trend patterns in SV during exercise are proven signs of cardiac function impairment (e.g. coronary artery disease). Another example: In critical care, fluid management is of paramount importance. Evolution and variation of SV are markers of fluid status and need, for instance during Passive Leg Raise test.
Very unfortunately CO has so far been underused because of the invasive, cumbersome and inaccurate nature of the available measurement techniques. Their cost has also been a limiting factor.
What makes a good CO measurement system ?
Ideally, a CO measuring system should be non invasive, easy to use, cost effective and of course accurate. Invasive techniques, although being generally considered accurate, clearly lack in the first three departments.
Non invasive techniques are generally considered to be less reliable. This vision belongs to the past and needs to be revised. A more comprehensive understanding of a CO device performance should encompass criteria such as reproducibility, sensibility and should take into full consideration the clinically significant margin of error of the so called "gold standards".
In reality, with a margin of error of 15 to 20%, reference techniques are clearly flawed. Indeed, a change in CO is considered being clinically significant starting with 15% (Pinsky. Why measure cardiac output? Critical Care, April 2003, 7:114-116 *). If one accepts a similar margin of error for the new technique (15%), even a difference in reading between the two techniques of as high as 30% (twice the clinical margin!) does not allow the operator to decide which device is right and which device is wrong (Critchley et al. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit, 1999, 15: 85-91 *).
If a real and near perfect "gold standard" CO measurement tool existed for validation purposes, it is not obvious that widely used CO methods such as Thermodilution would be accepted as valid today by the medical community, the more so as they are often operator dependent and variable.
Furthermore, the invasive nature of these techniques and the inherent risk associated with their use (often under estimated by the operators) result in questionable outcomes in terms of mortality and morbidity, as shown in some well known studies (Connors et al. The effectiveness of right heart catheterization in the initial care of critically ill patients. JAMA 276, 1996).
The reasonable doubt about the accuracy and safety of these invasive techniques and the direct and hidden costs associated with their use should pave the way for alternative noninvasive approaches. This process is unfortunately very slow precisely because of the widespread confusion between clinical standard and gold standard. One may even consider doubting the validity of the entire scientific literature describing studies comparing new methods to these questionable gold standards, to say the least.
In summary a new gold standard in CO measurement should feature:
- Reasonably correlated CO readings as compared with invasive references considering their intrinsic margin of error.
- Superior reproducibility and sensitivity has compared to invasive reference techniques.
- PhysioFlow has it all !
(*) These scientists are not users of PhysioFlow